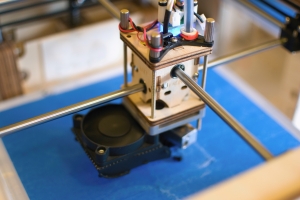
Three-dimensional (3-D) printed medical devices are becoming more common in the industry. Subtractive manufacturing, the more traditional method for a milled device, consists of starting with a block of material and removing different parts of the material in order to create the final device. The other common method is injection molding, which is ideal for high quantities of the same product type. The method used in 3-D printing, additive manufacturing, creates the product layer by layer, only using the necessary material. This innovative manufacturing technique provides many benefits including the ability to create patient-specific devices as well as intricate shapes and designs that are otherwise very difficult. However, these benefits do not come without regulatory challenges.
 Validating 3-D printed devices for sterilization requires flexibility and creativity. Because 3-D printed devices can be customized and are often patient specific, it is difficult to establish a set path for testing and validation. Traditional concepts of family grouping and batch testing are incorporated in a different way with these products. It is unlikely that entirely new validation approaches will need to be created as the principles will remain the same, however, existing validation processes will be modified to account for the additive manufacturing process and a batch size of one product.
Validating 3-D printed devices for sterilization requires flexibility and creativity. Because 3-D printed devices can be customized and are often patient specific, it is difficult to establish a set path for testing and validation. Traditional concepts of family grouping and batch testing are incorporated in a different way with these products. It is unlikely that entirely new validation approaches will need to be created as the principles will remain the same, however, existing validation processes will be modified to account for the additive manufacturing process and a batch size of one product.
In some cases a greater emphasis will be placed on process characterization and process validation rather than product testing. The current testing approaches for sterilization of medical devices primarily focus on the end product.
An example of changes which are made to typical approaches is in the bacterial endotoxins test (BET). BET is required for products which contact circulating blood and cerebral spinal fluid and is generally performed on three to 10 samples which are removed from every batch for testing. When the manufacturing batch size is one product, it is not possible to remove additional products from the batch for testing. It also seems unreasonable to require that for every patient-specific product manufactured, an additional three samples are manufactured for testing purposes. The current standards do allow for variations to the sample size, but it takes a knowledgeable microbiologist to properly rationalize a smaller sample size.
Another issue to consider, again in BET, is whether the sample or samples tested must be exactly the same configuration as the actual product. Some of the patient-specific products manufactured are complex and expensive. The question must be raised regarding whether it is appropriate and necessary to require that a company manufacture an exact replica of every patient-specific product for the BET. These products might take, for example, four hours to manufacture and be made of expensive materials. In this situation a rationale could be established which allows for manufacturing and testing of a surrogate product (e.g., a coupon) which is more reasonable in both time to manufacture and quantity of material. These options are also allowed in standards, but again, they require an experienced microbiologist to properly rationalize.
A reputable testing facility, such as Nelson Labs, employs knowledgeable microbiologists and expert consultants to help manufacturers achieve FDA approval for their 3-D printed medical devices. For more information or to schedule a consultation, contact Nelson Labs at 801-290-7502 or [email protected].